My posts are mostly about holistic health, wellness, and various methods to achieve balance in our lives. Human behavior or psychology are subjects I have delved deeper into, as our behavior dramatically affects our mental, physical, and spiritual well-being.
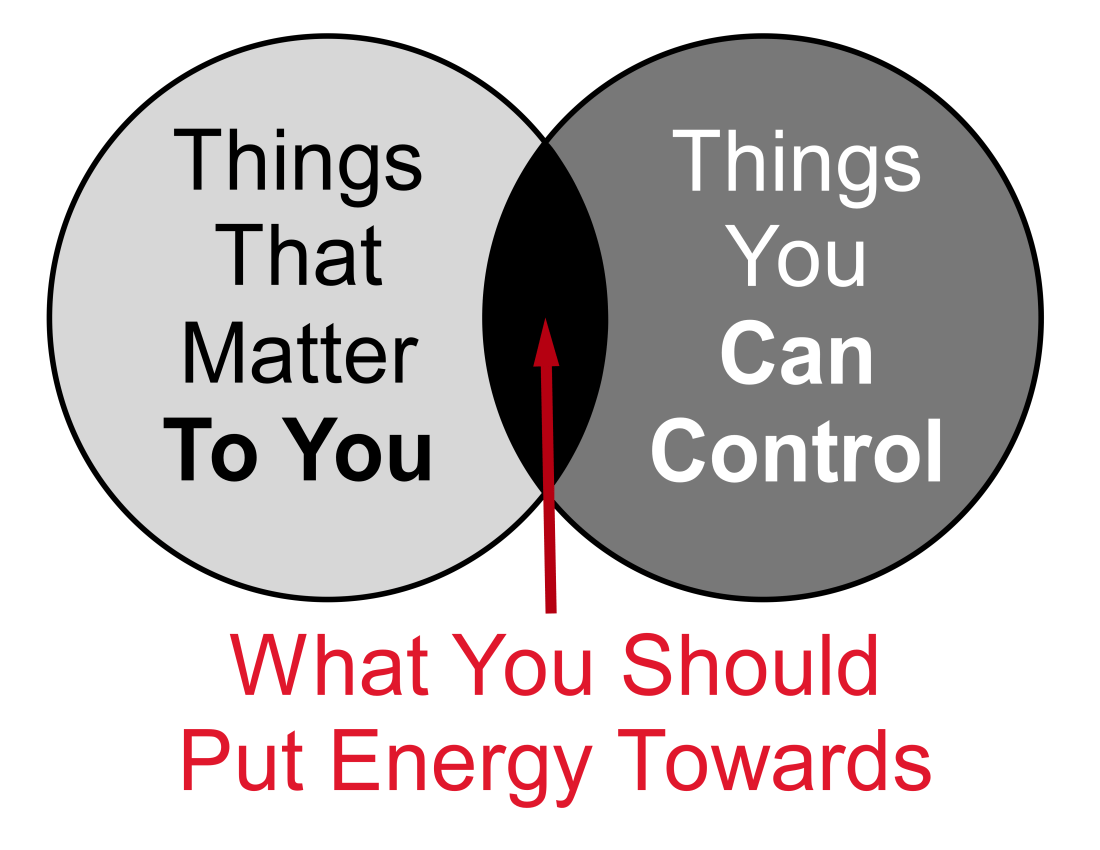
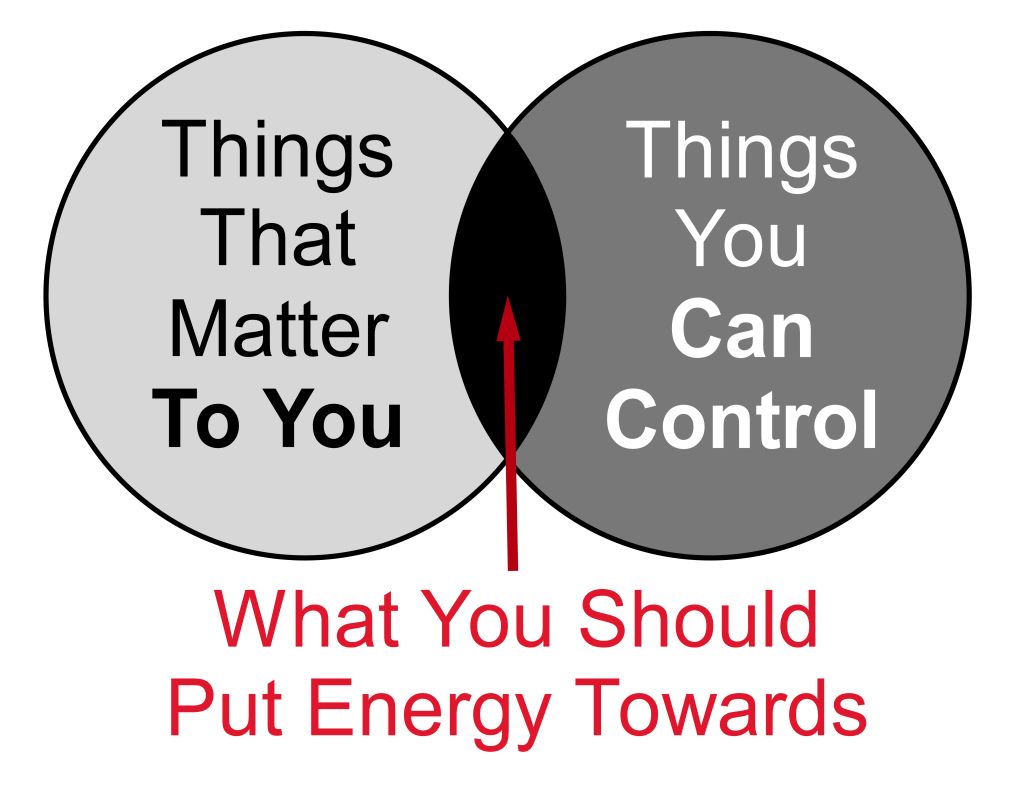
The United States is a nation built on ideals of freedom, opportunity, and justice, but beneath these principles lies a web of contradictions. Many Americans know systemic issues, broken systems, and political dysfunction, yet they often feel powerless to enact meaningful change. Some believe they have no viable alternatives, while others simply don’t care as long as the consequences don’t affect them directly. Lack of agency (ability to act and make choices independently) and lack of control (exerting power or influence over others or outcomes) can have deep psychological effects, leading to many chronic cognitive ailments such as depression, anxiety, insecurity, and others. It’s time for a collective reckoning. Perhaps it’s time to ask not just, “Are we part of the problem?” but also, “What can we do to be part of the solution?”
Here’s a closer look at some of the most glaring contradictions or cognitive dissonance (the discomfort of holding conflicting beliefs or values) in American society, grouped by their interrelated themes:
🏛️ Government and Political Dysfunction
1. Term Limits vs. Career Politicians
There is widespread support for imposing term limits on politicians, yet career politicians dominate Washington. Many Americans believe fresh perspectives would benefit governance, but efforts to enforce limits consistently stall. Voters complain about corruption but continue re-electing the same people.
2. Politicians and Insider Trading vs. Public Trust
Most Americans believe politicians should not benefit from insider trading, yet cases of elected officials profiting from privileged information persist. Despite this, the same politicians often get re-elected. We claim to detest corruption but keep endorsing those who abuse their positions.
3. Foreign Wars vs. Public Opinion
A large portion of the population opposes foreign military interventions, yet the U.S. remains entangled in conflicts worldwide. Public sentiment rarely translates into policy changes, highlighting the disconnect between the will of the people and government actions.
4. Perceived Misuse of Tax Dollars vs. Continued Compliance
Taxpayers express frustration over how their money is spent, with glaring examples of inefficiency and corruption. For instance, California spent $24 billion to address homelessness, yet the crisis has only worsened. In November 2024, the Pentagon failed to pass its annual audit, meaning that it wasn’t able to fully account for how its $824 billion budget was used. This was the 7th failed audit in a row, since the Department of Defense became required to undergo yearly audits in 2018. Despite this, people continue paying taxes while feeling powerless to demand accountability.
5. Daylight Saving Time vs. Public Opinion
Twice a year, Americans grumble about the disruption caused by changing the clocks. Studies show that daylight saving time may increase health risks and reduce productivity, yet it persists. Despite widespread dissatisfaction, legislative inertia keeps the practice alive.
6. Limited Political Choices vs. Frustration with the Two-Party System
Americans lament the lack of political diversity and the stranglehold of the two-party system, yet alternative parties remain marginalized. Even though many feel disillusioned, they continue to choose between the “lesser of two evils.” Real change remains elusive because the system favors the status quo.
💰 Economics and Consumer Behavior
7. Support for Public Education vs. Private School Enrollment
Public education is hailed as the cornerstone of equal opportunity, yet families who can afford it often opt for private schooling. This creates a disconnect between advocating for public education and personal choices that contribute to inequality.
8. Supporting Local Businesses vs. Shopping Online
We talk about the importance of supporting local businesses, yet giants like Amazon, Walmart, and Starbucks continue to dominate, often putting small businesses out of business. Convenience, competitive pricing, and free shipping lure consumers away from their local economies.
9. Income Inequality vs. Celebrity Worship
While many decry income inequality and the wealth gap, America remains obsessed with celebrity culture and extravagant lifestyles. This fascination with the ultra-wealthy perpetuates distorted perceptions of success and value.
10. Perceived Value vs. Price Sensitivity
Consumers often complain about the declining quality of goods and services but continue purchasing cheap, mass-produced items instead of supporting higher-quality alternatives. The desire for instant gratification and low prices outweighs long-term sustainability.
🏥 Health, Lifestyle, and Well-Being
11. Fast Food Consumption vs. Health Awareness
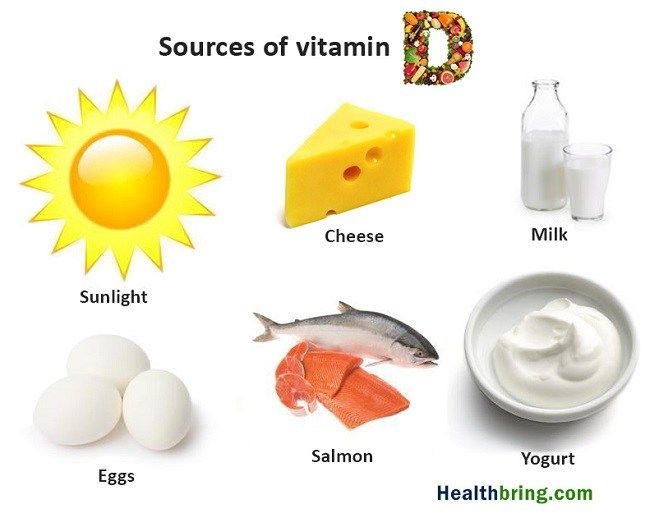
We know fast food is unhealthy. Obesity, diabetes, and other ailments continue to soar, yet fast-food chains thrive. Parents claim they care about their children’s health but often default to convenience, feeding them processed foods while allowing endless hours of screen time. Nutrition takes a backseat to ease, and the consequences are generational.
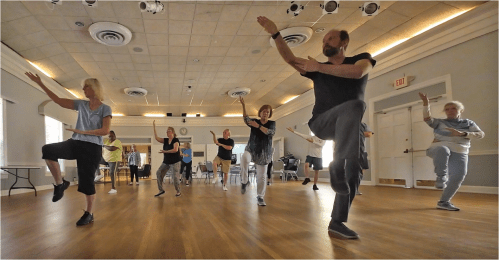
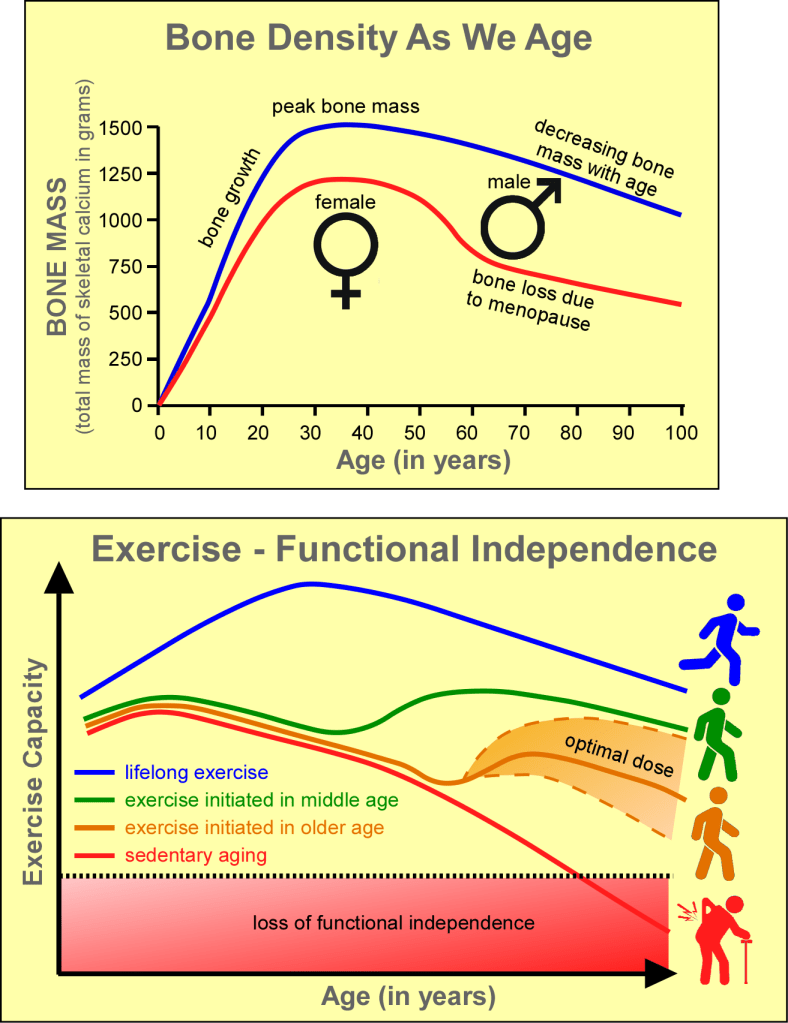
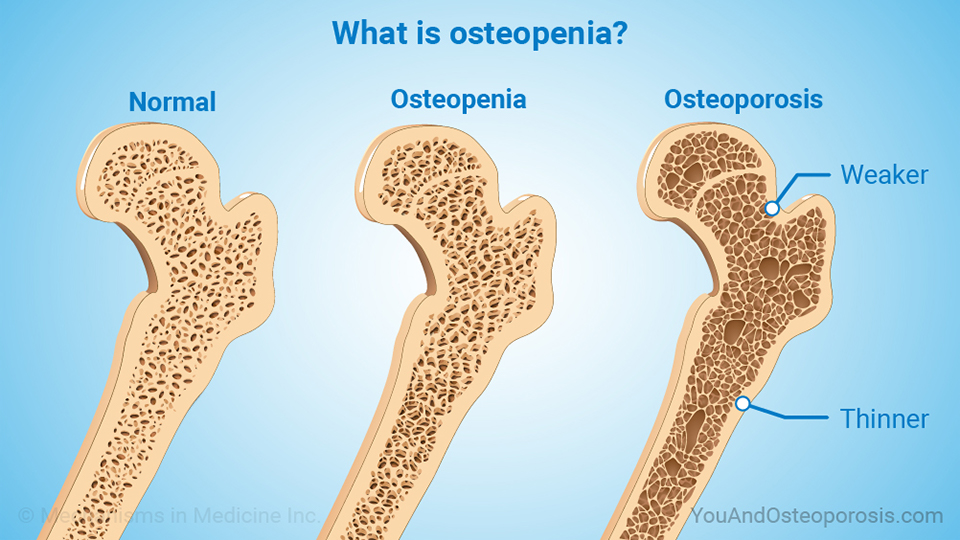
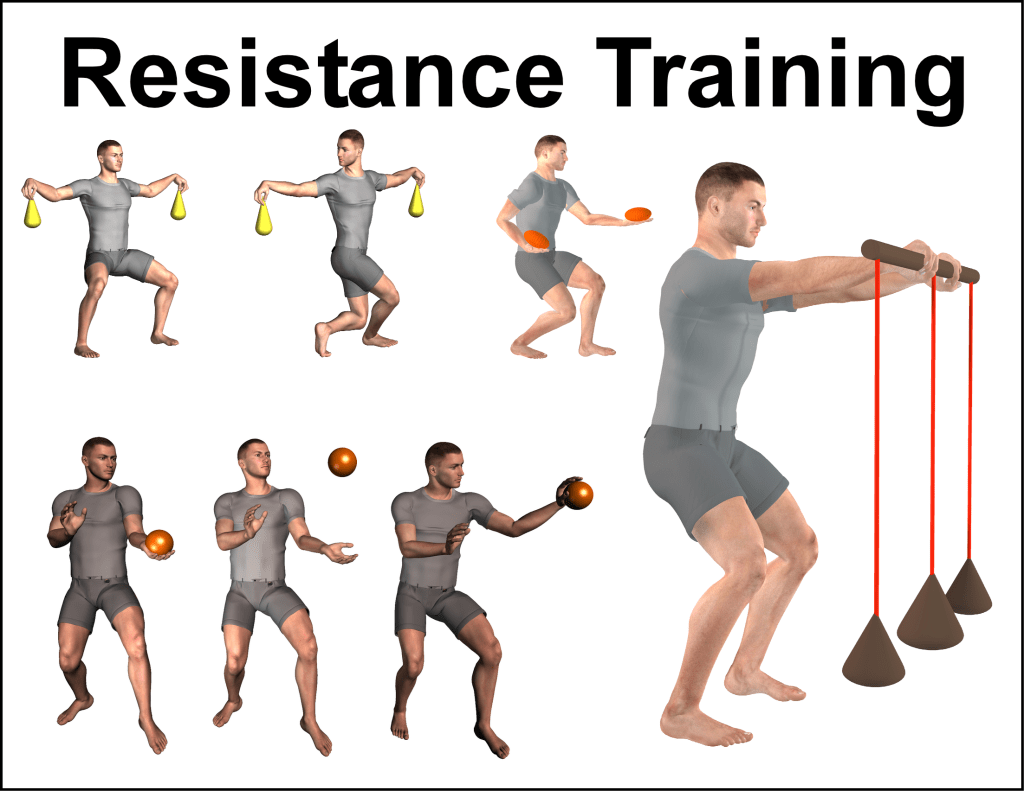
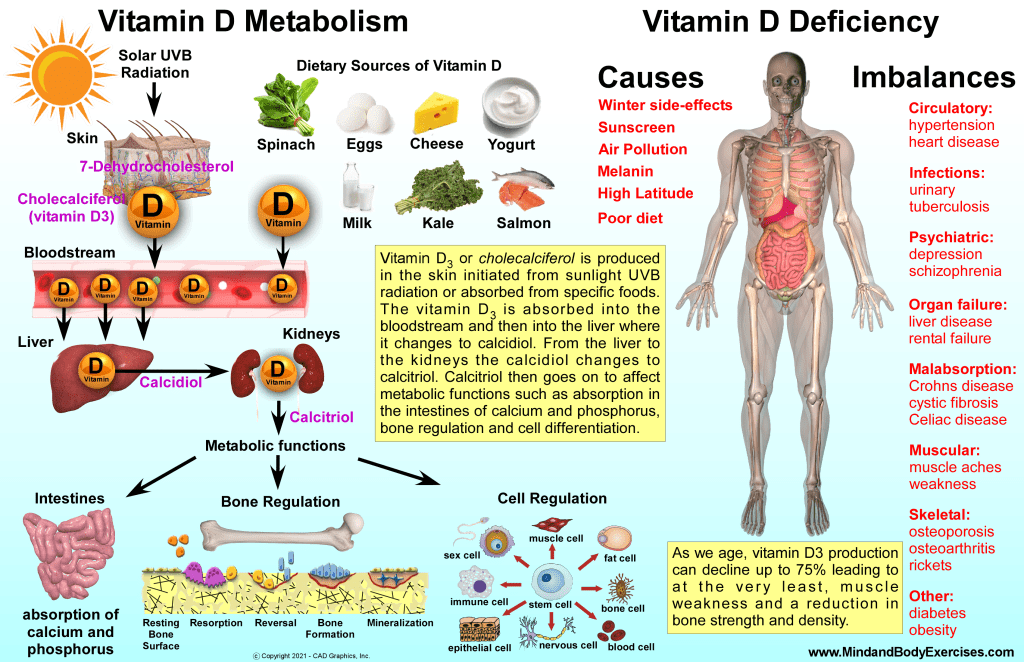
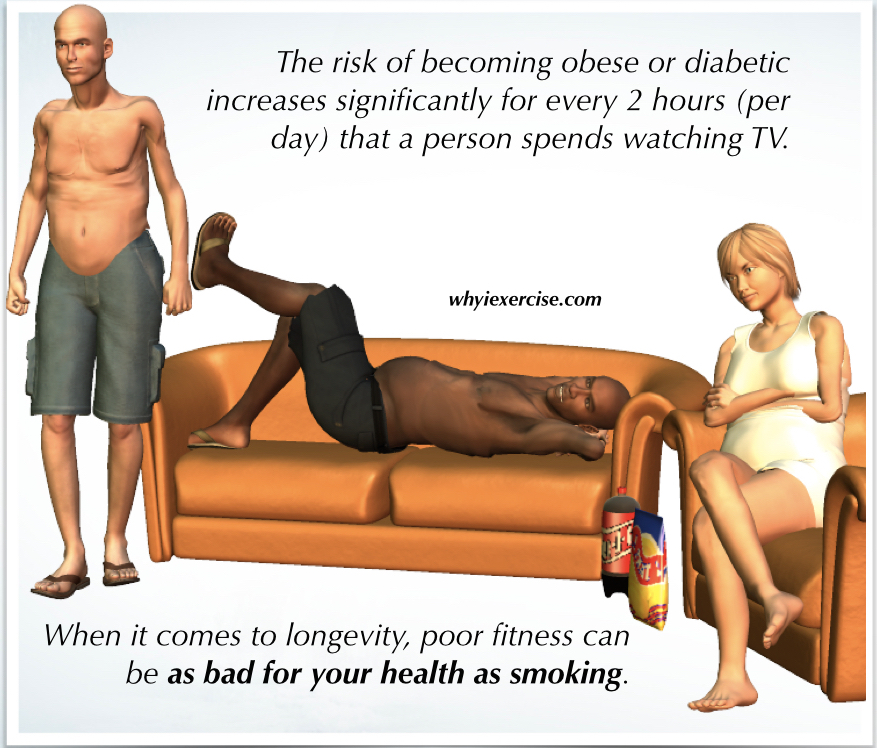
12. Sedentary Lifestyles vs. Advocacy for Healthy Living
We advocate for fitness, movement, and healthy living, yet modern lifestyles promote sedentary habits such as long hours at desks, excessive screen time, and minimal physical activity. Knowledge doesn’t always translate to action.
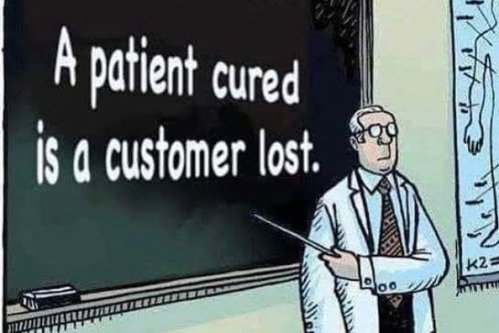
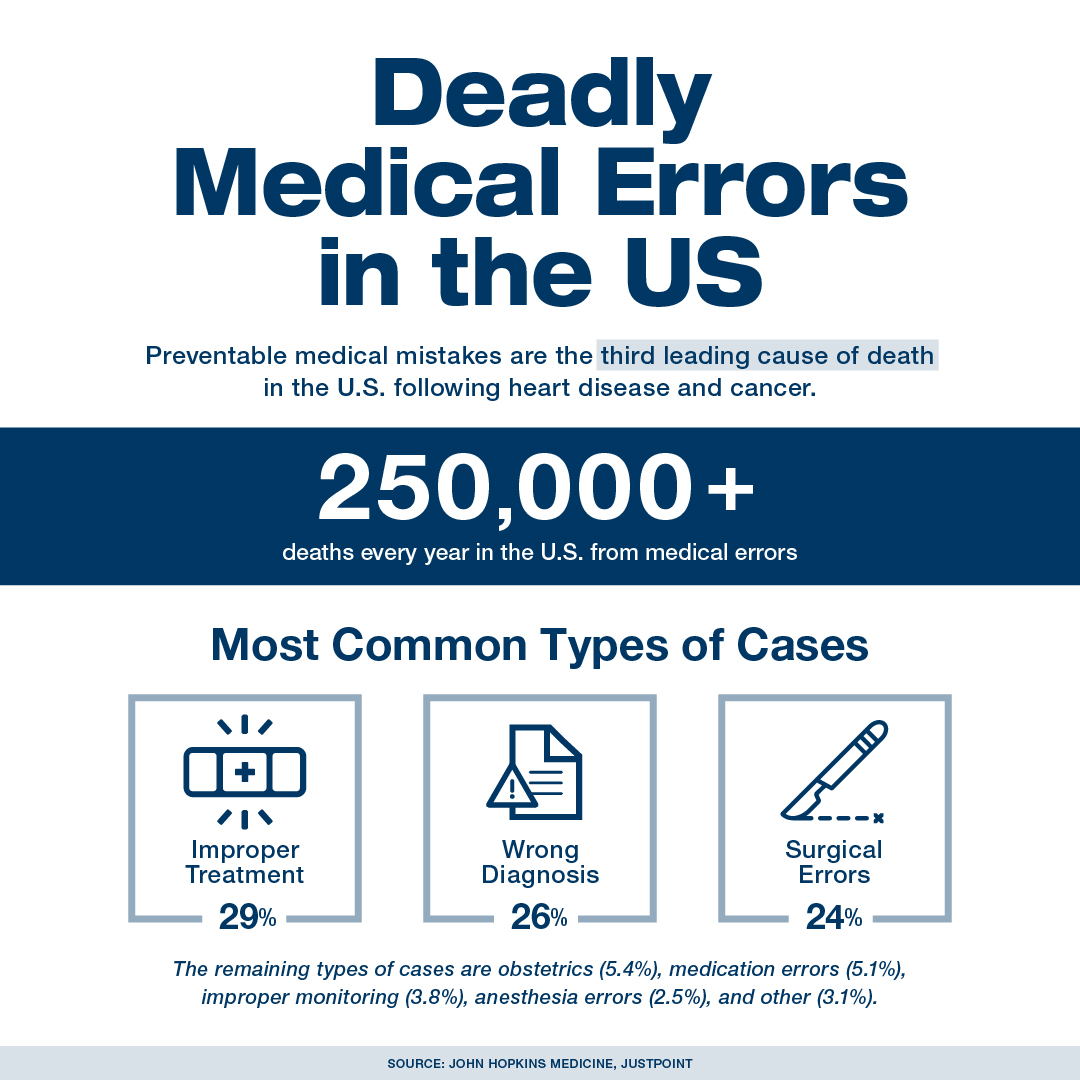
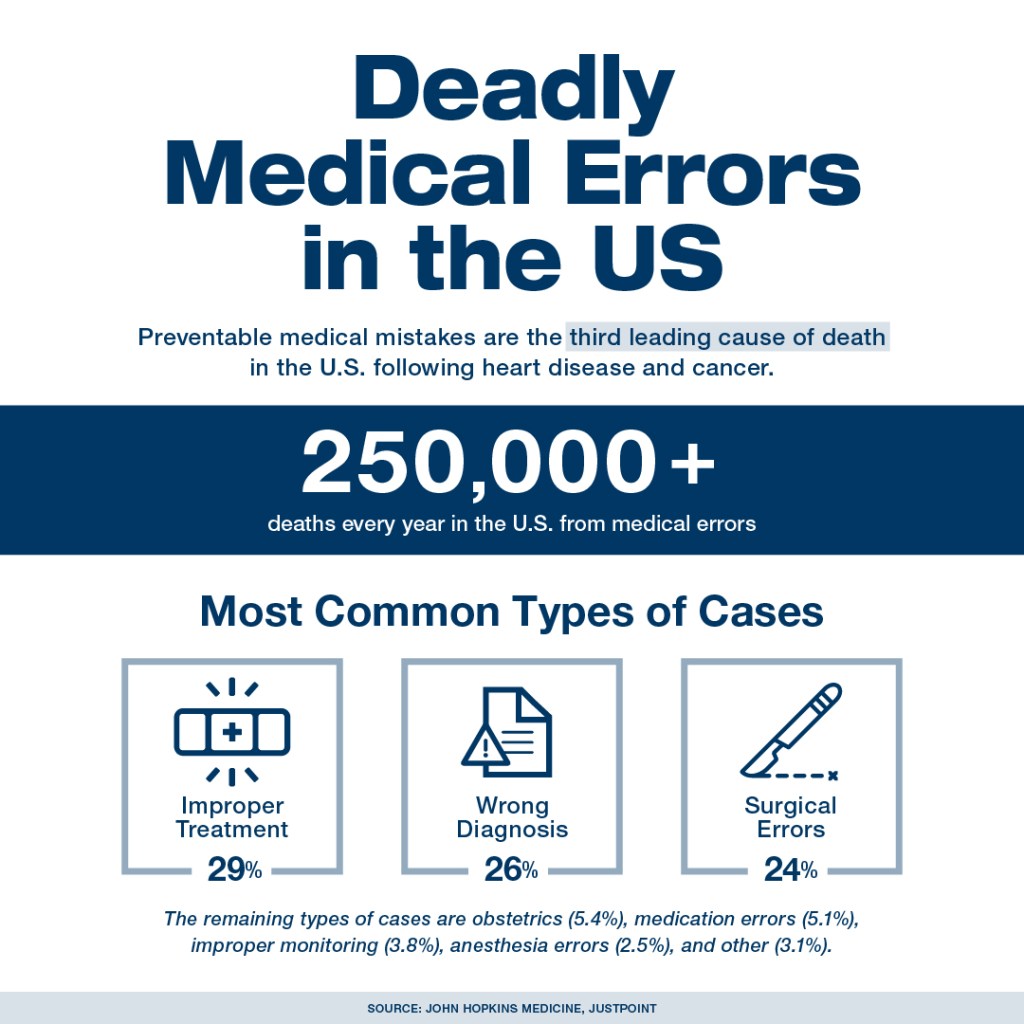
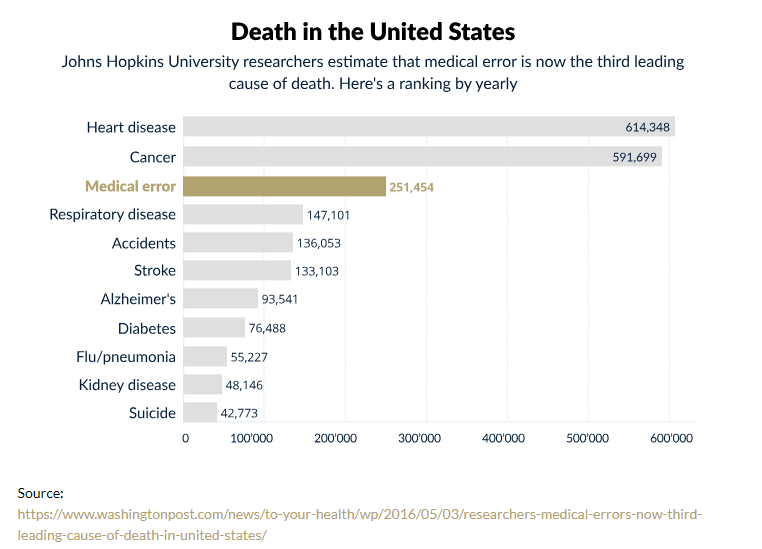
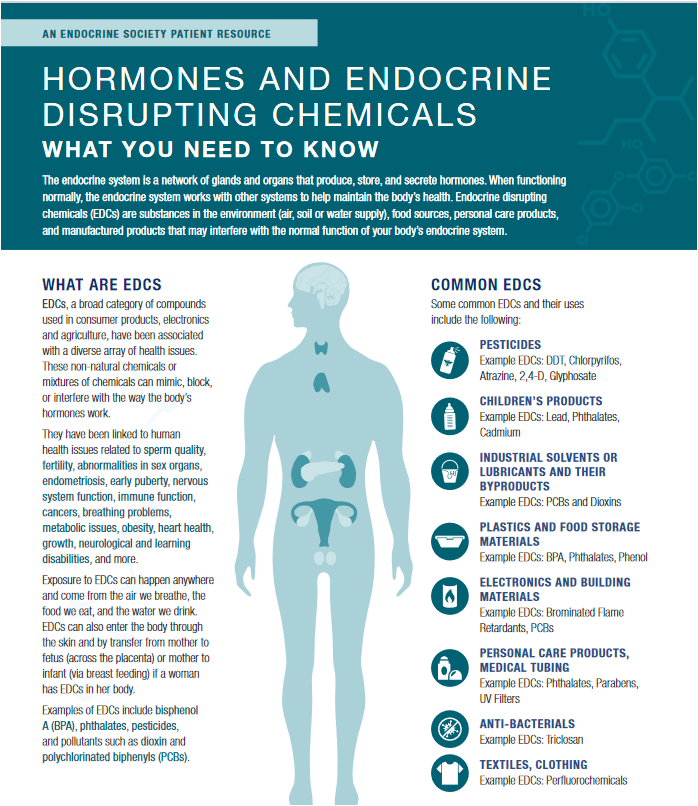
13. Healthcare System Criticism vs. Reliance on It
Americans recognize that the healthcare system is broken, yet they remain reliant on it. Pharmaceutical companies flood the media with advertisements, influencing consumers and doctors alike. Few healthcare professionals advocate for changes in lifestyle, diet, and exercise favoring “a pill for every ill.” The system favors profits over people, but viable alternatives are scarce, leaving many trapped in a cycle of dependency.
14. Body Positivity vs. Unrealistic Beauty Standards
The body positivity movement advocates for acceptance and inclusivity, but media, advertising, and Hollywood continue to promote unrealistic beauty standards. Thinness, youth, and perfection remain the ideal, perpetuating negative body image and self-esteem issues.
15. Desire for Work-Life Balance vs. Overworking Culture
Many Americans yearn for a better work-life balance, yet the culture of overwork persists. Long hours, limited vacation time, and a “hustle mentality” lead to burnout and mental health struggles. We value personal well-being in theory but often sacrifice it in practice.
🌎 Environment and Sustainability
16. Environmental Awareness vs. Consumerism
Many Americans express concern about climate change and environmental degradation but continue consuming at unsustainable levels. Convenience, affordability, and habit often override sustainable choices. The “Not in My Backyard” (NIMBY) mentality prevails, as people want solutions without altering their lifestyles.
17. Recycling Rhetoric vs. Minimal Action
Americans advocate for recycling and environmental protection, yet most recycling programs are underutilized or ineffective. Many items placed in recycling bins end up in landfills, and people often lack awareness of proper recycling practices.
🔒 Privacy, Technology, and Social Isolation
18. Privacy Concerns vs. Social Media Addiction
Many express concerns over privacy and data security in the digital age, yet millions willingly share intimate details of their lives on platforms that harvest personal data. We fear surveillance but continue scrolling, liking, and posting. Convenience and entertainment often outweigh the fear of losing control over our private information.
19. Spam, Telemarketers, and Privacy Violations vs. Acceptance of Invasions
Americans complain about the relentless onslaught of spam calls, telemarketers, and digital intrusions, yet many accept these invasions as a normal part of modern life. We express frustration over privacy violations but rarely take steps to secure our information or demand accountability from corporations that exploit personal data.
20. Community Engagement vs. Social Isolation
Americans value community engagement and connection, yet the rise of digital communication and urbanization has led to increased social isolation. We crave connection but often retreat into virtual worlds, losing the sense of belonging that real communities provide. We see electronic devices as babysitters for children and adults alike, and then wonder why so many are depressed, anxious, and unable to be comfortable in real-life social settings.
21. Mistrust of Big Tech vs. Dependence on It
Americans frequently express mistrust of big tech companies, citing concerns about monopolies, privacy, and censorship. Yet, dependence on platforms like Google, Facebook, and Amazon remains pervasive. We resent their power but rely on their convenience.
⚖️ Ethics, Morality, and Social Justice
22. Human Rights Advocacy vs. Selective Outrage
Many advocate for human rights and justice but remain selective in their outrage, often influenced by political affiliations or cultural biases. Genuine concern for equality should transcend partisanship, yet inconsistencies persist.
23. Religious Values vs. Material Pursuits
America prides itself on being a nation of faith, yet materialism and consumerism often overshadow spiritual values. Many profess religious beliefs but prioritize wealth, status, and success over moral and ethical principles.
24. Public Demand for Change vs. Fear of Disruption
Perhaps the most significant contradiction is that while Americans express a desire for change, they also fear the disruption that change may bring. Breaking free from familiar systems requires effort, sacrifice, and discomfort—something many are unwilling to endure.
🪶 Historical Amnesia and Disregard for the Marginalized
25. The Forgotten Victims: Native Americans and Historical Amnesia
America celebrates its history of freedom and democracy while ignoring the ongoing consequences of genocide and displacement inflicted on Native American communities. Treaties were broken, lands were stolen, and entire cultures were nearly erased. Yet, mainstream narratives often gloss over these atrocities, perpetuating historical amnesia. The plight of Native Americans remains a footnote in history books, even as they continue to face systemic inequalities.
26. Advocacy for Social Justice vs. Ignoring Indigenous Struggles
While advocating for social justice and equality, many overlook the ongoing struggles of indigenous communities. Issues such as land sovereignty, environmental degradation, and broken treaties remain unresolved, highlighting a glaring inconsistency in America’s commitment to justice.
🔍 A Nation at a Crossroads
America’s contradictions are not just individual dilemmas—they reflect the collective psyche of a nation grappling with competing values and desires. To move forward, we must confront these inconsistencies with honesty and courage. True change starts not just by acknowledging these contradictions but by taking deliberate action to align our values with our behavior. “Change the world!” “Fix the system!”
Instead: Are we ready to face the mirror? How about changing ourselves?
I look forward to further sharing more of my message by partnering with hospitals, wellness centers, VA centers, schools on all levels, businesses, and individuals who see the value in building a stronger nation through building a healthier population.
I also have hundreds of FREE education video classes, lectures, and seminars available on my YouTube channel at:
https://www.youtube.com/c/MindandBodyExercises
Many of my publications can be found on Amazon at:
http://www.Amazon.com/author/jimmoltzan
My holistic health blog is available at:
https://mindandbodyexercises.wordpress.com/
http://www.MindAndBodyExercises.com
Mind and Body Exercises on Google: https://posts.gle/aD47Qo
Jim Moltzan
407-234-0119