The Perception of Healthy Eating as a Privilege in the U.S. Healthcare Landscape
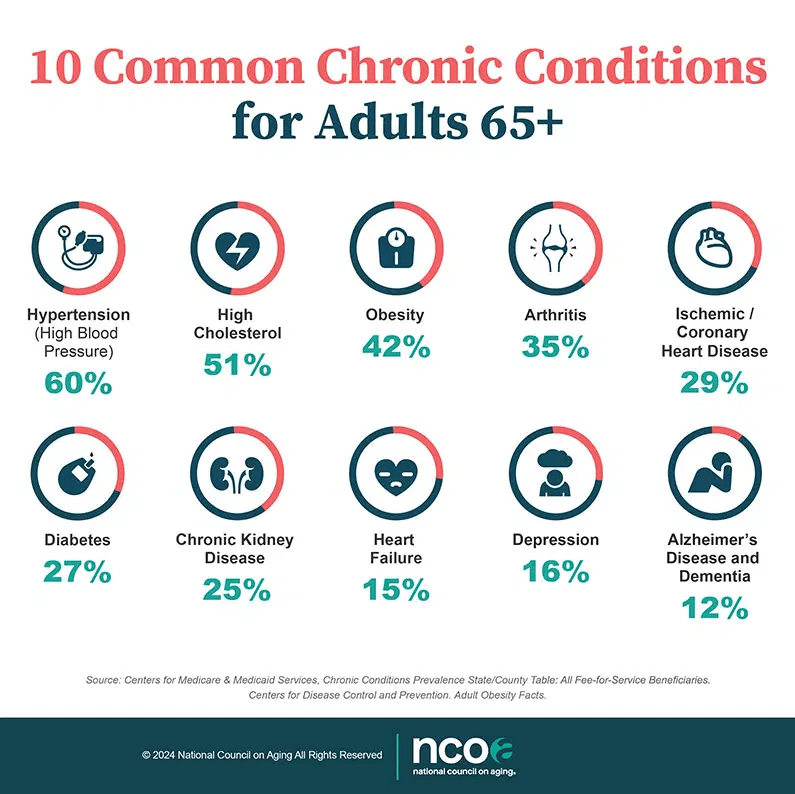
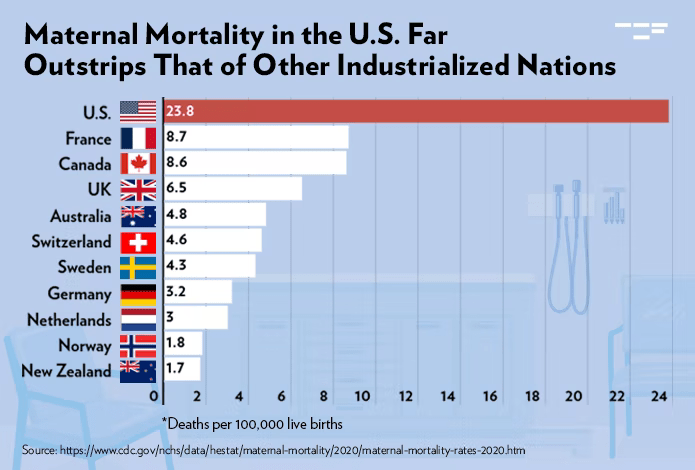
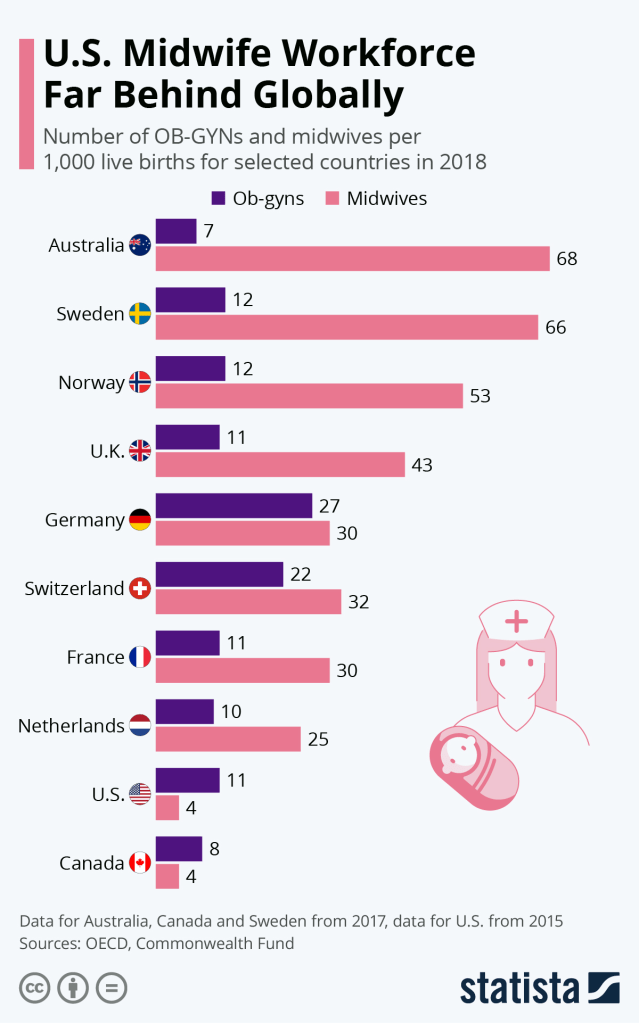
Today in the US, access to nutritious food is often perceived as a privilege rather than a basic necessity. There is a combination of systemic issues in the food and healthcare industries, social inequality, and perhaps a narrow public understanding of just what good health consists of. These issues have contributed to driving up the cost of nutritious food, creating significant obstacles to maintaining a healthy balanced diet. Ironically, as US healthcare costs continue to rise dramatically, the consumption of unhealthy foods contributes to chronic health conditions creating a vicious circle of events that push individuals further into the healthcare system and consequently perpetuating the cycle of preventable diseases. These are factors that in the US, have shaped the perception that eating healthfully is a luxury and how this perception stems from economic, cultural, and educational factors that influence food choices, physical health, and overall well-being.
Economic Constraints: Why Healthy Food Costs More
A simple reason for the perception of healthy eating as a luxury is the cost disparity between purchasing of nutritious and non-nutritious foods. Organic, fresh, and minimally processed foods are typically more expensive due to significant factors such as agricultural practices, supply chain logistics, and governmental subsidies (Ver Ploeg et al., 2015). Organic farming methods are more labor-intensive and produce lower crop yields compared to of conventional farming, which relies more heavily on use of chemical pesticides and fertilizers (Hughner et al., 2007). This added labor cost, along with a limited supply, increases the cost of organic food, making it less accessible to individuals with lower incomes (Ver Ploeg et al., 2015). Conversely, crops like soy, corn, and wheat, which are often genetically modified and treated with chemicals, are heavily subsidized by the U.S. government, making processed foods derived from these crops less expensive for consumers. This economic landscape perpetuates a cycle where affordable, nutritionally poor food is more accessible, while healthier options remain financially out of reach.
Processed Foods: The Price of Convenience
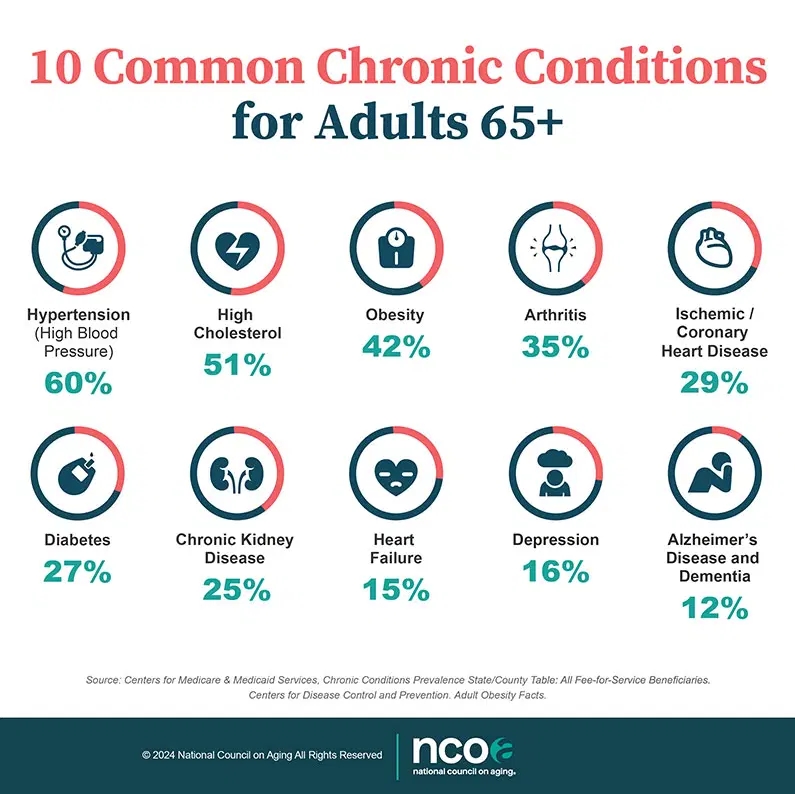
Aside from cost, processed foods that are loaded with sweeteners, artificial preservatives, and flavor enhancers are designed for maximum taste appeal, convenience, and shelf stability. These foods are quite often high in sugars, salt, and unhealthy fats, all of which contribute to obesity, diabetes, and cardiovascular disease (Monteiro et al., 2018). Low-income neighborhoods, where grocery stores lack fresh produce, frequently rely on this calorie-dense but nutritionally lacking products. The convenience and affordability of these foods cloud the fact that they are contributors to poor health when consumed long-term. The perception that eating healthy is a privilege, reflects not only the cost of food but also the accessibility and desire for unhealthful options that fit into the American fast-paced, budget-conscious lifestyles (Ver Ploeg et al., 2015).
Education and Health Literacy: The Hidden Barrier
A major factor adding to this issue is a lack of health education and literacy among the general population. Understanding the impact of nutrition on long-term health is not prioritized in many US schools, and misinformation about what constitutes “healthy” is extensive (Nestle, 2013). Marketing campaigns often mislead consumers into thinking that “sugar-free” or “low-fat” foods are healthy. In reality, these foods often contain harmful additives like high-fructose corn syrup or aspartame, which both have been linked to various health risks (Swithers, 2015). Also, public knowledge of the role of whole foods, hydration, and balanced macronutrient intake is often dismal, leading some to make choices that encourage immediate taste satisfaction over long-term health benefits (Nestle, 2013). As a result, the cultural perception of healthful food as a luxury is partly fueled by a lack of nutritional knowledge, leading individuals to turn to less expensive, popular foods over healthier, less well-understood options.
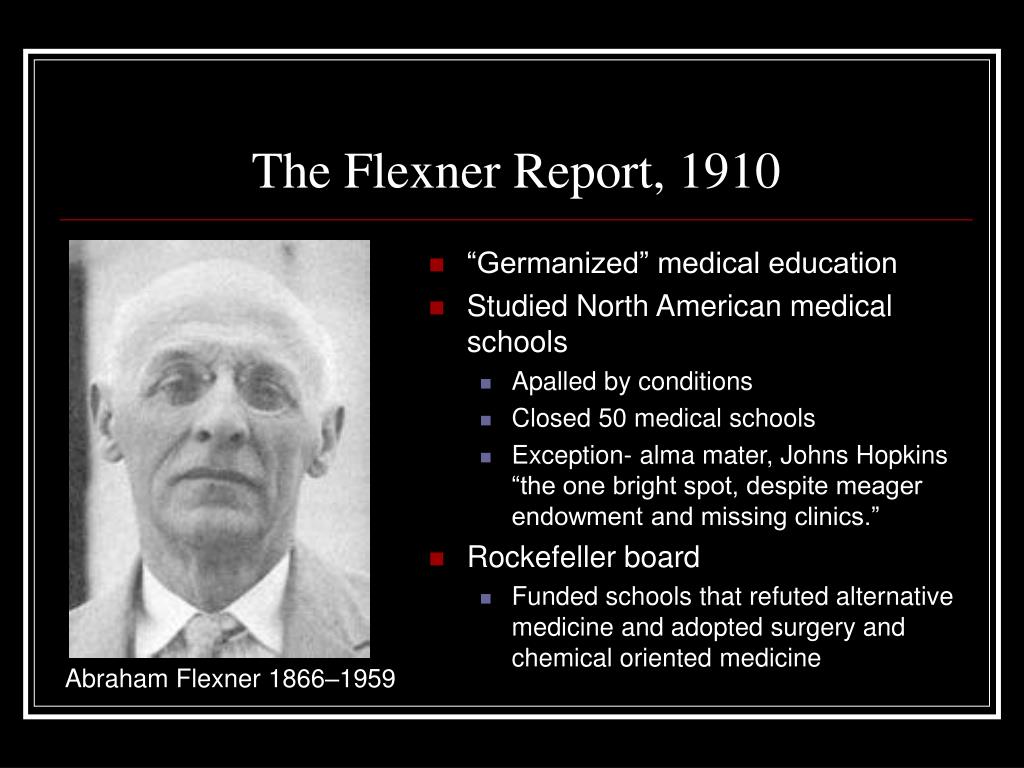
The Institutional Influence: Schools and Healthcare
Schools and the healthcare system also shape public perception and access to healthy food. School meal programs, specifically those in lower-income areas, often offer highly processed foods due to budget constraints and limited resources for fresh ingredients (Gaines et al., 2014). This reinforces the idea that nutrient-dense foods are exceptional rather than essential. Just as the U.S. healthcare system prioritizes treatment over prevention, schools rarely encourage dietary education as part of comprehensive healthcare (Schroeder, 2007). While medical professionals widely recognize the link between diet and chronic disease, the system rarely encourages preventive approaches, including education relative to nutrition and lifestyle changes (Schroeder, 2007). This gap leaves many young Americans, especially those without access to nutritional education, without a clear understanding of how a healthy diet influences long-term health.
Bottled Water vs. Sugary Beverages: A Reflection of Misplaced Priorities
The fact that bottled water costs more than soda and soft drinks reflects the prioritization of profit over public health. Soda and other sugary beverages are relatively cheap due to subsidies for their ingredients and widespread production. Bottled water prices remain high due to packaging and branding processes. This pricing paradox encourages consumers, particularly those with limited resources to choose soda over water. The strategic marketing of sugary drinks as less-expensive alternatives further contributes to poor dietary habits and supports the idea that basic, healthy choices are a privilege for the exclusive or elitist.
Breaking the Cycle: A Call for Systemic Change
Recognizing and addressing the perception of having a healthy diet, being a privilege requires systemic changes across multiple sectors. Lawmakers must evaluate agricultural subsidies to level the playing field between nutrient-dense foods and heavily processed products (Miller et al., 2016). Schools should encourage nutritional education and pursue methods to improve food quality within budgetary limits, especially in low-income areas (Gaines et al., 2014). Additionally, healthcare providers should encourage preventive care practices that focus on dietary education, empowering patients to make more informed food choices. With these changes, healthy eating can become more accessible and implemented.
In conclusion, the view of healthy eating as a luxury reflects societal inequities within the American food and healthcare systems. By reducing economic and informational barriers to nutritious food, American society can cultivate a culture where healthy choices are more available to everyone, making better health and well-being, not a privilege but a shared right.
References
Gaines, A. B., Lonis-Shumate, S. R., & Gropper, S. S. (2011). Evaluation of Alabama public school wellness policies and state school mandates. Journal of School Health, 81(5), 281-287. https://doi.org/10.1111/j.1746-1561.2011.00588.x
Hughner, R. S., McDonagh, P., Prothero, A., Shultz, C. J., & Stanton, J. (2007). Who are organic food consumers? A compilation and review of why people purchase organic food. Journal of Consumer Behaviour, 6(2-3), 94-110. https://doi.org/10.1002/cb.210
Monteiro, C. A., Cannon, G., Levy, R. B., Moubarac, J.-C., Jaime, P., Martins, A. P., … & Swinburn, B. (2018). Ultra-processed foods: What they are and how to identify them. Public Health Nutrition, 21(1), 6-8. https://doi.org/10.1017/S1368980018003762
NESTLE, M. (2013). Food Politics: How the Food Industry Influences Nutrition and Health (1st ed.). University of California Press. http://www.jstor.org/stable/10.1525/j.ctt7zw29z
Schroeder, S. A. (2007). We can do better—improving the health of the American people. New England Journal of Medicine, 357(12), 1221-1228. https://doi.org/10.1056/NEJMsa073350
Swithers, S. E. (2015). Artificial sweeteners are not the answer to childhood obesity. Appetite, 93, 85-90. https://doi.org/10.1016/j.appet.2015.03.027
Ver Ploeg, M., Mancino, L., Todd, J. E., Clay, D. M., & Scharadin, B. (2015). Where do Americans usually shop for food and how do they travel to get there? Initial findings from the National Household Food Acquisition and Purchase Survey. U.S. Department of Agriculture, Economic Research Service.
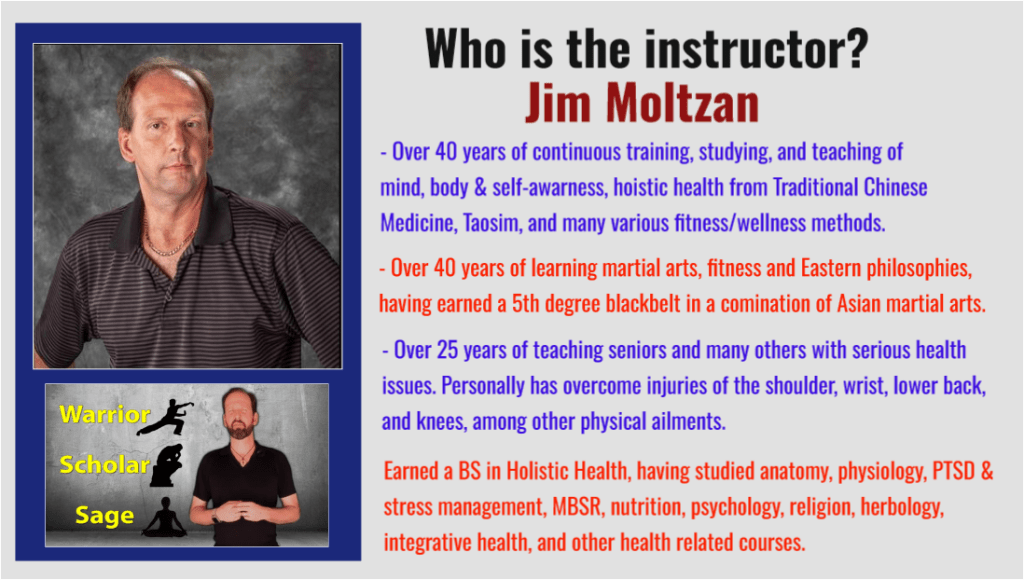
I teach and offer lectures about holistic health, physical fitness, stress management, human behavior, meditation, phytotherapy (herbs), music for healing, self-massage (acupressure), Daoyin (yoga), qigong, tai chi, and baguazhang.
Please contact me if you, your business, organization, or group might be interested in hosting me to speak on a wide range of topics related to better health, fitness, and well-being.
I look forward to further sharing my message by partnering with hospitals, wellness centers, VA centers, schools on all levels, businesses, and individuals who see the value in building a stronger nation through a healthier population.
I also have hundreds of FREE education video classes, lectures, and seminars available on my YouTube channel at:
https://www.youtube.com/c/MindandBodyExercises
Many of my publications can be found on Amazon at:
http://www.Amazon.com/author/jimmoltzan
My holistic health blog is available at:
https://mindandbodyexercises.wordpress.com/
http://www.MindAndBodyExercises.com
Mind and Body Exercises on Google: https://posts.gle/aD47Qo
Jim Moltzan