Despite living in an age of advanced medicine and rising health awareness, chronic illness, emotional suffering, and addiction continue to rise. This contradiction invites us to question not just our treatments but also the mindset and motivations behind them. Increasingly, research and lived experience point to unprocessed pain and trauma as the core drivers of both psychological and physiological illness.
Medicine’s Narrow Focus: Suppressing Symptoms Instead of Healing
Contemporary medical practices often focus on symptom suppression rather than root-cause healing. For example, elevated cortisol, a hormone associated with stress, is frequently managed with pharmaceuticals that reduce inflammation but fail to address the underlying source of distress (Sapolsky, 2004). In cases of chronic illness, especially cancer, mainstream interventions often fall back on drastic methods: cutting (surgery), poisoning (chemotherapy), or burning (radiation), with minimal inquiry into psychosomatic or emotional contributors.
The pharmaceutical industry has also come under scrutiny for prioritizing profit-driven solutions that treat stress biochemically without offering tools for actual emotional or relational healing (Gabor Maté, 2010).
A Society Obsessed with Health Yet Unwell
We live in a paradoxical society: obsessed with fitness, diet, and health optimization, yet disconnected from authentic well-being. Emotional pain is frequently seen as a personal failure, and expressions of vulnerability are often equated with weakness. Shame becomes a hidden driver of behavior, shaping identity through internalized messages like “I’m not enough” or “My needs don’t matter” (Brown, 2012).
The metaphor of the “monster” within, like the transformation of Bruce Banner into the Hulk, illustrates how repressed emotions can erupt when unacknowledged. We often assume that other people’s issues are about us, leading to further internal conflict and disconnection.
Trauma: The Root Cause of Addiction and Illness
Pain, especially unresolved emotional pain, is at the root of many afflictions. According to trauma expert Gabor Maté (2008), addiction is not a disease or choice but a response to deep suffering. Whether through substances, work, food, or achievement, people are often trying to soothe pain they may not even fully understand.
Social disconnection, abandonment, and lack of emotional education perpetuate trauma across generations. Society offers little support or guidance for managing grief, shame, or stress. Many turn to coping mechanisms without the tools to process their trauma, which is especially evident in marginalized communities where chronic stress is linked to disproportionately higher rates of illness (Williams & Mohammed, 2009).
The Cost of Disconnection and the Need for Authenticity
In professional fields like medicine, unresolved trauma is common. Some individuals pursue high-achieving careers not from passion but to compensate for feelings of inadequacy or unlovability. Emotional detachment, often a survival strategy in childhood, becomes normalized in adulthood. This disconnection between mind and body leads to chronic stress, illness, and burnout (Van der Kolk, 2014).
Authentic healing requires honoring two essential human needs: attachment and authenticity. When these needs are in conflict, as they often are in trauma survivors, authenticity is usually sacrificed for the sake of relational survival. Reconnecting with one’s truth, expressing anger constructively, and embracing emotional honesty are key steps toward transformation.
Healing the Generational Wounds
Trauma doesn’t disappear. It is often passed from one generation to the next, not just through genetics but through behavior, belief systems, and emotional suppression. Children absorb the stress of their caregivers. Without awareness and intervention, these patterns replicate over time (Yehuda & Lehrner, 2018).
What may appear as weakness, in hypervigilance, dissociation, emotional volatility, is often a response to longstanding unmet needs. Healing begins by naming these patterns and allowing space for expression and integration.
A Shift Toward Integration and Compassion
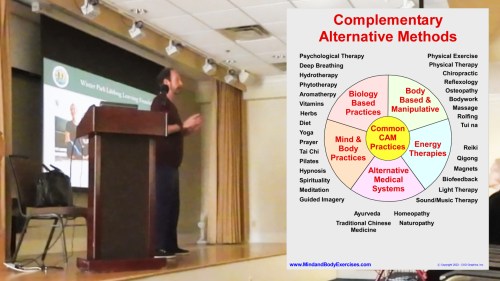
The healing path is not just clinical, it is relational, emotional, and spiritual. Psychedelic-assisted therapy, somatic practices, plant medicines like ayahuasca, and trauma-informed psychotherapy are gaining traction because they center empathy, connection, and emotional truth (Carhart-Harris & Goodwin, 2017).
As we reevaluate addiction, trauma, and illness through this lens, we begin to see that these challenges are not signs of brokenness. Rather, they are indicators of what needs acknowledgment, healing, and reintegration. Addiction, far from being a moral failure or inherited defect, can be seen as a solution to an emotional problem, a cry for help that must be understood before it can be addressed.
References
Brown, B. (2012). DARING GREATLY. In GOTHAM BOOKS. GOTHAM BOOKS. https://site.ieee.org/sb-nhce/files/2021/06/Brene-brown-book1.pdf
Carhart-Harris, R. L., & Goodwin, G. M. (2017). The therapeutic potential of psychedelic drugs: Past, present, and future. Neuropsychopharmacology, 42(11), 2105–2113. https://doi.org/10.1038/npp.2017.84
Maté, G. (2008). In the realm of hungry ghosts: Close encounters with addiction. Knopf Canada. https://drgabormate.com/book/in-the-realm-of-hungry-ghosts/
Maté, G. (2010). When the body says no: The cost of hidden stress. Wiley. When the Body Says No – Dr. Gabor Maté
Sapolsky, R. (2004). Why Zebras don’t get Ulcers: The acclaimed Guide to Stress, Stress-Related Diseases, and Coping. ResearchGate. https://www.researchgate.net/publication/272161275_Why_Zebras_Don’t_Get_Ulcers_The_Acclaimed_Guide_to_Stress_Stress-Related_Diseases_and_Coping
Van der Kolk, B. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking. The body keeps the score: Brain, mind, and body in the healing of trauma.
Williams, D. R., & Mohammed, S. A. (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32(1), 20–47. https://doi.org/10.1007/s10865-008-9185-0
Yehuda, R., & Lehrner, A. (2018). Intergenerational transmission of trauma effects: Putative role of epigenetic mechanisms. World Psychiatry, 17(3), 243–257. https://doi.org/10.1002/wps.20568